(NewsNation) — More than 600,000 Americans are expected to die of cancer in 2022 — an outcome often the result of a delayed diagnosis. That’s particularly true for lung cancer, accounting for one in four cancer deaths.
“Although the statistics are decreasing, (lung cancer) is still the largest cause of cancer-related deaths worldwide,” said Dr. Janani Reisenauer, a thoracic surgeon and an interventional pulmonologist. “Most of the time, people don’t notice any symptoms until it’s much later in their stage and it’s harder to treat.”
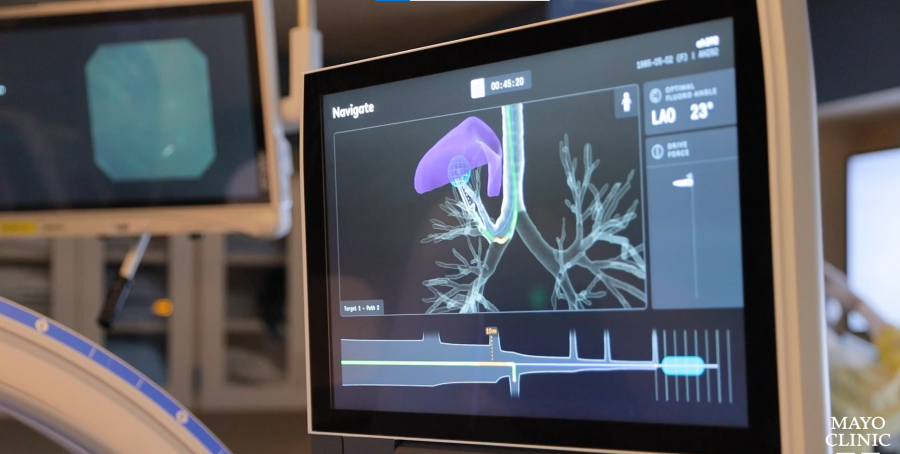
Robotic bronchoscopy, a procedure where the doctor uses a tiny robotic arm to go into the air passages of the lungs and take a biopsy, is aiming to change that.
Reisenauer was one of the first in the nation to test this technology during clinical trials at the Mayo Clinic, beginning in 2019. Their research shows this method is more accurate, can reach further into the lungs and has fewer complications.
“Knowing that the statistics are what they are, if we can figure out how to stop (lung) cancer in its tracks, it has profound implications for the population as a whole,” she said.
NewsNation spoke with Reisenauer about the promise of robotic bronchoscopy to prevent deaths and change the way cancer is treated.
This interview has been edited for length and clarity.
NewsNation: Why is this technology so revolutionary?
Reisenauer: Robotic bronchoscopy essentially is a tiny, three-millimeter scope that can be driven anywhere in the lung.
We can reach almost 98-99% of all nodules, where the old bronchoscopes could maybe only get to nodules about 40% of the time. We’re able to sample and accurately provide a diagnostic result, whether that’s cancer or not, about 85-92% of the time. That’s in contrast to the previous data, which ranged anywhere from 20% to about 70%.
In addition, complications of severe or significant bleeding is very low, less than 1%. And then the pneumothorax (lung collapse) rate is also exceedingly low, less than 1%.
NewsNation: What are some of the challenges with traditional bronchoscopy?
Reisenauer: Prior to this, bronchoscopic biopsies were with larger bronchoscopes. Only lesions that were pretty central, or pretty close to an airway, or kind of larger in size, were those that we would even attempt (to biopsy).
Right now, this device is only meant to go down your windpipe and your airways and your airway tubes. But it definitely brings about an interesting opportunity in terms of other technologies that can be made to go through other parts of the body.
NewsNation: But it’s not just being small enough to travel through the airways of the lungs — it’s that you can see where you’re going, right?
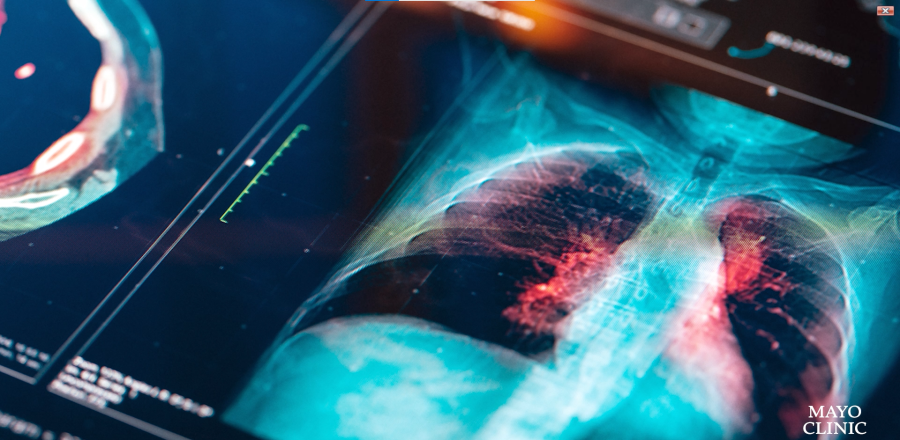
Reisenauer: Imaging has become very advanced as well. What we’re using now is a combination of a portable CT scanner in conjunction with these robotic bronchoscopes. These not only allow you to see where you are inside the lung, but see where you are relative to other critical structures.
That allows us to make sure that we’re actually sampling in the nodule — and not next to or beside the nodule, potentially leading to a false result.
I’m a thoracic surgeon as well. And many times under video guidance, these nodules are difficult to see. These catheters allow us to tattoo lesions so that we can see them at the time of the resection.

NewsNation: How could similar technology not just prevent but treat cancer?
Reisenauer: There’s endless potential in terms of what this technology will allow us to do.
There are opportunities to look at injection of drugs — as opposed to having to give somebody drugs through the vein — potentially injecting it focally and avoiding the systemic toxicities and the side effects. There may be opportunities to kill the tumor cells with extreme heat or extreme cold or other energy methods. There’s been a lot of news about immunotherapy, targeted therapies and therapies based on genetic mutations and molecular markers.
Being able to treat somebody focally — who maybe isn’t healthy enough to tolerate something going into their veins, or is too sick for chemotherapy — there’s tremendous implications for that. And it’s just having another tool in your toolkit.

